- The fetal blood reaches the placenta via the umbilical arteries, which are branches of the caudal aortic system. Well-oxygenated blood from the placenta is returned by the umbilical veins, about one-half passing through the liver sinusoids, and the rest bypassing the liver via the ductus venosus into the inferior vena cava system. The blood flow is regulated by a muscular sphincter in the ductus venosus, close to the umbilical veins. The blood then passes to the right atrium. Since the inferior vena cava also receives deoxygenated blood from the lower portion of the body, the blood entering the right atrium is not as well oxygenated as that in the umbilical veins
- The minor circulation (circulation through the lungs): although existing anatomically, the minor circulation is almost completely short-circuited by 2 major mechanisms
- THE BLOOD FROM THE INFERIOR VENA CAVA is directed largely by the lower border of the septum secundum, through the foramen ovale, which directs blood from the right to the left side of the heart. Here it mixes with small amounts of deoxygenated blood returning from the lungs via the pulmonary veins
- From the left atrium, blood goes to the left ventricle and out of the heart via the aorta to vessels of the head and neck, upper limbs, and the rest of the body. The former receive richer, well-oxygenated blood
- Some oxygenated blood from the inferior vena cava stays in the right atrium, mixes with deoxygenated blood from the superior vena cava and coronary sinus, and passes to the right ventricl Blood leaves via the pulmonary trunk and passes through the ductus arteriosus, which diverts it from the pulmonary to the aortic system
- Little goes to the lungs (?10%) due to pulmonary vascular resistance
- The mixed blood in the descending aorta (58% saturated with oxygen) passes to the umbilical arteries and is returned to the placenta for reoxygenation
- THE FETUS cannot use its pulmonary system since it lives in a liquid environment. The lungs, nevertheless, have been ready and prepared to fulfill their role from month 6 of pregnancy. It becomes effectively functional only when the fetus is born
- Circulation at birth: placental circulation is interrupted. The abrupt drop in intrathoracic pressure brought about by the first respiration (aeration of the lungs) helps contribute to the initial pulmonary circulation
- BLOOD PRESSURE decreases in the pulmonary artery even though its flow is increased since it supplies a capillary network considerably enlarged by expansion of the pulmonary parenchyma
- As a result, blood flow decreases (even reverses momentarily) in the ductus arteriosus; its walls contract, and in a few days, it closes off completely
- Closure appears to be mediated bybradykinin, released from the lungs during their initial inflation. Its action depends on the high oxygen content of the aortic blood resulting from ventilation of the lungs at birth
- Similarly, influx of pulmonary blood into the left atrium causes the septum primum to be pressed against the septum secundum, and the foramen ovale is closed
- The umbilical arteries also constrict at birth and prevent blood loss
- THE CIRCULATORY SYSTEM at this time-resembles its adult form, with separation of the minor and major circulations. Nevertheless, occlusion of the 2 circuits is still, for some time, only physiologic (functional)
- THE CIRCULATORY SYSTEM becomes fully anatomic after several weeks due to the proliferation of endothelial and fibrous tissue
- Fibrous degeneration of the ductus arteriosus forms the ligamentum arteriosum, between the left pulmonary artery and the concave inferior surface of the aortic arch
- Complete fusion of the septum primum to the septum secundum forms a definitive interatrial septum. Traces of the former passage, the foramen ovale, are seen as a depression, the fossa ovalis, in the right interatrial wall.
- The fetal blood reaches the placenta via the umbilical arteries, which are branches of the caudal aortic system. Well-oxygenated blood from the placenta is returned by the umbilical veins, about one-half passing through the liver sinusoids, and the rest bypassing the liver via the ductus venosus into the inferior vena cava system. The blood flow is regulated by a muscular sphincter in the ductus venosus, close to the umbilical veins. The blood then passes to the right atrium. Since the inferior vena cava also receives deoxygenated blood from the lower portion of the body, the blood entering the right atrium is not as well oxygenated as that in the umbilical veins
- The minor circulation (circulation through the lungs): although existing anatomically, the minor circulation is almost completely short-circuited by 2 major mechanisms
- THE BLOOD FROM THE INFERIOR VENA CAVA is directed largely by the lower border of the septum secundum, through the foramen ovale, which directs blood from the right to the left side of the heart. Here it mixes with small amounts of deoxygenated blood returning from the lungs via the pulmonary veins
- From the left atrium, blood goes to the left ventricle and out of the heart via the aorta to vessels of the head and neck, upper limbs, and the rest of the body. The former receive richer, well-oxygenated blood
- Some oxygenated blood from the inferior vena cava stays in the right atrium, mixes with deoxygenated blood from the superior vena cava and coronary sinus, and passes to the right ventricl Blood leaves via the pulmonary trunk and passes through the ductus arteriosus, which diverts it from the pulmonary to the aortic system
- Little goes to the lungs (?10%) due to pulmonary vascular resistance
- The mixed blood in the descending aorta (58% saturated with oxygen) passes to the umbilical arteries and is returned to the placenta for reoxygenation
- THE FETUS cannot use its pulmonary system since it lives in a liquid environment. The lungs, nevertheless, have been ready and prepared to fulfill their role from month 6 of pregnancy. It becomes effectively functional only when the fetus is born
- Circulation at birth: placental circulation is interrupted. The abrupt drop in intrathoracic pressure brought about by the first respiration (aeration of the lungs) helps contribute to the initial pulmonary circulation
- BLOOD PRESSURE decreases in the pulmonary artery even though its flow is increased since it supplies a capillary network considerably enlarged by expansion of the pulmonary parenchyma
- As a result, blood flow decreases (even reverses momentarily) in the ductus arteriosus; its walls contract, and in a few days, it closes off completely
- Closure appears to be mediated bybradykinin, released from the lungs during their initial inflation. Its action depends on the high oxygen content of the aortic blood resulting from ventilation of the lungs at birth
- Similarly, influx of pulmonary blood into the left atrium causes the septum primum to be pressed against the septum secundum, and the foramen ovale is closed
- The umbilical arteries also constrict at birth and prevent blood loss
- THE CIRCULATORY SYSTEM at this time-resembles its adult form, with separation of the minor and major circulations. Nevertheless, occlusion of the 2 circuits is still, for some time, only physiologic (functional)
- THE CIRCULATORY SYSTEM becomes fully anatomic after several weeks due to the proliferation of endothelial and fibrous tissue
- Fibrous degeneration of the ductus arteriosus forms the ligamentum arteriosum, between the left pulmonary artery and the concave inferior surface of the aortic arch
- Complete fusion of the septum primum to the septum secundum forms a definitive interatrial septum. Traces of the former passage, the foramen ovale, are seen as a depression, the fossa ovalis, in the right interatrial wall.

Thursday, April 13, 2017
Embryology: Circulation of blood before and after birth. By: Anmol Advani
Wednesday, April 12, 2017
Arches of Foot By Geeta goswami.
What is arch?
Longitudinal(i-e Sagittal plane) and transverse (i-e Frontal and hhorizontal planes) concavity of foot profile maintained by interlocking shapes of bones, plantar ligaments(i-e ligaments in the sole of the foot), plantar aponeurosis(plantar fasciai-e the thick connective tissue present on plantar side of the foot), tendons of extrinsic muscles and tension imposed by intrinsic muscle action.Bones involve in arches formation:
Tarsals bone: Metatarsals bone:
1)-Talus. 1st (medial) MT bone.
2)-Calcaneus. 3rd MT bone.
3)-Navicular bone. . 4th MT bone.
4)-Cuboid. 5th MT bone.
Plantar ligaments forming arches of Foot:
1)-Plantar plates.
2)-Metatarsal and tarsometatarsal ligaments.
3)-Long plantar ligament.
4)-Plantar calcaneocuboidal ligament.
5)-Plantar calcaneonavicular ligament.
6)-Plantar cuneonavicular ligament.
7)-Plantar intercuniform ligament.
8)-Plantar cuboideonavicular ligament.
9)-Plantar cuneocuboid ligament.
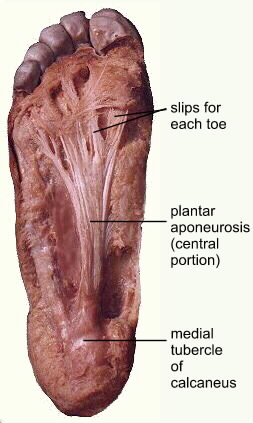
Planter aponeurosis:
Types of arches:
a) Longitudinal:
1. Medial.2. Lateral.
b) Transverse:
1. Anterrior.
2. Posterior.
Formation or structure of Arches:
Medial longitudinal Arch:
This arch is considerably higher, more mobile & resilient than the lateral. Its constitution isisas follows.Ends:
The anterior end is formed by the heads of the first, second and third metatarsals. The phalanges do not take part in forming the arches. The posterior end of this arch is formed by the medial tubercle of the calcaneum.
Summit:
The summit of the arch is formed by the superior articular surface of the body of the talus.Pillars:
The anterior pillar is long and weak.It is formed by the talus, the navicular, the three cuneiform bones, and the first three metatarsal bones. Posterior pillar is short and strong. It is formed by the medial part of the calcaneum.The major joint of the arch is the tarsocalcaneonavicular joint.
Lateral longitudinal Arch:
This arch is characteristically low, has limited mobility, & is built to transmit weight and thurst to the ground. This is in contrast to the medial longitudinal arch which act as a shock absorber. The constitution of the lateral longitudinal arch is as follows.
Ends:
The anterior end of the arch is formed by the headhead of the 4th & 5thth Metatarsal bones. TheThe Posterior end is formed by the lateral tubercle of the calcaneum.
Summit:
The summit lies at the level of the articular facets on the superior surface of the calcaneum at the level of the subtalar joint.
Pillars:
The anterior pillar is long and weak. It is formed by the cuboidcuboid bone and by the 4th and 5th metatarsals. The posterior pillar is short and strong. It is formed by the lateral half of the calcaneum.
Main joint:
The main joint of the arch is the calcaneocubiod joint.
Anterior Transverse Arch:
The anterior transverse arch is formed by the heads of the five metatarsal bones. It is complete because the heads of the first and fifth metatarsals both come in contact with the ground, and form the two ends of the arch.
Posterior Transverse Arch:
The posterior transverse arch is formed by the greater parts of the tarsus & metatarsus. It is incomplete because only the lateral end comes in contact with the ground, the arch forming a 'half dome' which is cmplete by a silimar half dome of the opposite foot.
Factors Responsible For Maintenance Of Arches:
In general, the factors helping in maintaining the various arches areare as follows.
1. Shape of the bones concerned.
2. Intersegmental ties or ligaments (and muscles) that hold the different segments of the arch together.
3. Tie bones or bowstrings that connect the two ends of the arch.
4. Slings that leep the summit of the arch pulled up. Each of these factors is considered below.
1. Bony Factor:
The posterior transverse arch is formed, and maintained mainly because of the fact that many of the tarsal bones involved (e.g. the cuneiform bones) and the heads of the metatarsal bones, are wedge-shaped, the apex of the wedge pointing downwards.
The bony factor is not very important in the case of the other arches.
2. Intersegmental Ties:
All arches are supported by the ligaments uniting the bones concerned. The most important of these are as follows.
(I) The spring ligament for the medial longitudinal arch.
(II) The long and short plantar ligaments for the lateral longitudinal arch.
(III) In the case of the transverse arch, thethe Metatarsal bones are held together by the interrosseous muscles also.
3. Tie Beam:
The longitudinal arches are prevented from flattening the plantar aponeurosis, and by the muscles of first layer of the sole. These structures keep the anterior and posterior ends of these arches pulled together. In case of the transverse arch, the adductor hallucis acts as a tie beam.
4. Slings:
a) The summit of the medial longitudinal arch is pulled upwards by tendons passing from the posterior comparment of the leg into the sole, I.e.tibialistibialis Posterior, flexor hallucis longus, flexor digitorum longus.
b) The summit of the lateral longitudinal arch is pulled upwards by the peroneus longus & peroneus brevis.
c) The tendons of tibialis anterior and peroneus longus together form a sling(or stirrup) which keeps the middle of the foot pulled upwards, thus supporting the longitudinal arches.
d) As the tendon of the peroneus longus runs transversely across the solesole, it pulls the medial and lateral margins of the sole closer together, thus maintaining the transverse arches. The transverse arch is also supported by tibialis posterior which grips many of the bones of the sole through its slips.
What is the function of Arches?
Arches of foot help in:
1)-Weight- bearing.
2)-Providing upright posture.
3)-Fast walking.
4)-Running.
5)-Jumping.
NOTE:-Foot print are not complete due to the arches.
Wednesday, March 29, 2017
HUMAN EMBRYOLOGY~ BY MAHEK NOOR DAUDPOTA~
HUMAN
EMBRYOLOGY
• Human embryo-genesis is the process of CELL DIVISION
and cellular differentiation of the embryo that occurs during the early
stages of development.
• In
biological term, human development entails growth from a one-celled ZYGOTE to
an adult HUMAN BEING.
• Fertilization
occurs when the SPERM cell successfully
enters and fuse with an EGG CELL (Ovum).
• The
genetic material of the sperm and the egg then combine to from a single cell
called ZYGOTE and the germinal stage of prental development commence.
• Embryogenesis
cover the first eight week of development at the beginning of the ninth week
the embryo is termed a FETUS.
The human embryology is the study of this
development during first eight week after fertilization. The normal period of gestation (Pregnancy) is nine month or 38
weeks
• The
germinal stage refers to the time from fertilization through the development of
the early embryo until implantation is completed in the UTERUS.
• The
germinal stage takes around 10 days. During this stage, the zygote being to
divide, in a process called CLEAVAGE.
• A
BLASTOCYST is then formed and implanted in uterus.
• Embryogenesis
continues with the next stage gastrulation, when the three germ layers of
embryo from in the process called Histogenesis, and processes of Neurulation
and Organogenesis follow.
• In
comparison to the embryo, the fetus has more recognizable external features and more complete set of developing
organ. The entire process of embryogenesis involves coordinated spatial and
temporal changes in gene expression cell growth and cellular differentiation
• A
nearly identical process occurs in species, specially among chordates.

• Step
2: the first 12 to 24 hours after a zygote is formed are spent in cleavage –
very rapid cell division
• Step
3: during blastulation, the mass of cells from a hollow ball.
• Step
4: cell begin to differentiate and from cavities.
• Step
5a: the primitive streak forms.
Step 6: The notochord is formed
Neurulation
• Step
6a: tubes from, making neurula.
• Step
6b: the notochord induces the formation of the neural plate
• Step
6c: the neural plate folds in on itself to make the neural tube and neural
crest.
• Step
7: the mesoderm has five distinct categories.
Major Developmental Stages Of Embryonic Period (1-8thweek)
|
Time period (Week)
|
Major Events/characteristics
|
|
1st week
|
Fertilization, cleavage, morula formed (3days), blastocyst
superficially implanted, zona pellucida disappears, inner cell
mass(embryoblast)& outer cell mass(trophoblast) present. A cuboidal layer
of hypoblast is formed.
|
|
2nd week
|
Blastocyst enlarged, completion of implantation, formation of
amniotic cavity, yolk sac, extra-embryonic mesoderm, extra-embryonic coelom
that later become chorionic cavity. Bilaminar disc (ectoderm, endoderm) is
formed along with syncytiotrophoblast and cytotrophoblast. Primary chorionic
villi appear.
|
|
3rd week
|
Appearance of:- trilaminar
disc(ectoderm,mesoderm,endoderm), primitive streak(15 day), somites,
interembryonic mesoderm, notochord neural tube,body cavities cardiovascular
system
|
|
4th week
|
Body is narrow, tubular & C shaped limb buds appear,
appearance of four pair of branchial arches, placenta begins to form, heart
begins to beat, lens placodes and otic placodes formed, head & tail folds
present . Three primary brain vesicles also formed
|
|
5th week
|
Head increases greatly in size, face formed, limb buds shows
limbs, & upper limb become paddle shaped
|
|
6th week
|
Head dominant. Oral and nasal cavities confluent. Curvature of
embryo diminished. Digital rays, footplate, finger & toes recognizable
|
|
7th week
|
Yolk sac is reduced to yolk stalk and limb differentiate rapidly.
|
|
8th week
|
Head nearly as large as rest of the body. Genital tubercle formed
but sex difference is not obvious. Facial features are distinct. Eyes
directed more anteriorly. Neck is established, digits of hands and feet
seprated along with retrogression of tail.
|
Major Developmental Stages Of Embryonic Period (9-38th
weeks)
|
Time period (Week)
|
Major Events/characteristics
|
|
9-12th week
|
Rapid growth in fetal length, head still realtively large, eyes
look anteriorly, eyelids fused, lanugo & nails present. Primary
ossification centers appear.
|
|
13-16th week
|
Further rapid growth in fetal length, head still relatively large,
eyes widely separated but eyelids fused. External ears on side of head. Fetus
look human and sex recognition possible.
|
|
17-20th week
|
Lanugo covers entire body. Venix caseosa present. Hairs present on
head mother Quickening brown fat forms. Eyebrows and eye lashes present.
|
|
21-25th week
|
Skin wrinkled and red, head still relatively large, face child
like, fingers & toe nail develop. Interalveolar walls of lungs secrete
surfactant(24th week)
|
|
26-29th week
|
Skin wrinkles lost due to subcutaneous fats, eyelids open, hairs
on head longer, CNS matured and controlled breathing movement primitive
alveoli formed.
|
|
30-34th week
|
Skin is pink & smooth, langugo hairs has disappeared from
face. Vernix caseosa thick. Nails reach end of fingers.
|
|
35-38th week
|
Fetus fully developed, lanugo hairs disappear, nails project
beyond ends of finger and toes. Testis reachs scrotum.
|
|
266 days from conception
|
Birth
|
Friday, March 24, 2017
The Muscular System.......BY Aveenash
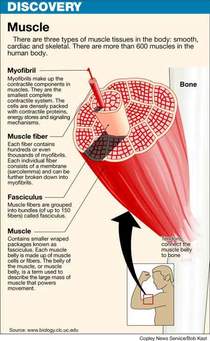
THE MUSCULAR SYSTEM
OUR MUSCLES
- Enable us to move our body parts.
- Give us to our individual shape.
- Protect and keep in place our abdominal organs.
- Enable to us good posture.
- Help in our circulation of blood.
- Generate body heat when contract.
- .
TYPES OF MUSCLES
Skeletal muscles
Smooth Muscles
Cardiac Muscles
1: Skeletal or Voluntary Muscles:
- They are under our conscious control.
- Attached to skeleton by Tendons.
- Causes movement of bones at joints.
- they are fatigue.
- Perform every day action such as: walking, runing, jumping.
The major Skeletal Muscles:
- Deltoid, Biceps, Abdominals (4 muscles), Quadriceps (4 muscles), Pectorals, Latisimus dorsi, Trapizius, Triceps, Gluteals (3 muscles), Hamstrings (3 muscles), gastrocnemius.
2: Smooth or Involuntary Muscles:
- These Muscles work automatically- they are not our under consciuos control.
- Example: Muscles of Digestive System.
-
3: Cardiac Muscles:
- Cardiac muscles are special type of involuntary muscles.
- It is only foundst in Heart.
- It contracts regularly, continuosly and without tiring.
- It works automatically but is under constant Nervous and Chemical control.
- .
HOW DO OUR MUSCLES WORK?
- There are 3 main types of muscular contraction:
Isotonic and Concentric
Isotonic and Eccentric
Isometric
Isotonic and Concentric: Our muscles shorten as the contract.
- Example: The bicep during a pull-up.
- Most Sporting Movements are this type.
Isotonic and Eccentric: Our muscles lengthen as they contract under tension.
- Example: The bicep when we lower down from a pull-up.
Isometric: Our muscles stay the same length as they contract.
- There is no movement , so the ends of muscles stay the same distance apart.
- Example: Our Shoulder Muscles during a tug of war.
- .
MUSCLES CAN WORK AS:
- Flexors: Contracting to bend our joints.
- Extensors: Contracting to straighten joints
. - Prime moovers (Agonists): Contracting to start a movement.
- Antagonists: Relaxing to allow movement to take place.
- Fixators: contracting to give the working muscles a firm base.
- Synergists: Stablising the area around the prime mover and fine tuning our movement.
MOVEMENT OF MUSCLES:
- Origin: The attachement of muscles to the bone that remains stationary.
- Insertion: The attachement of muscle to the bone that moves.
- Belly: The fleshy part of muscle between the tendons of origin and/ or insertion..
Muscles Disorders, Diseases and Injuries:
1: CRAMPS:
Involve sudden and violent muscles contractions. A person may experience painful cramps of certain skeletal muscles and smooth muscles.
2: MUSCLE SORENESS/Muscle strain:
Hard muscular may cause skeletal muscles become sore. In severe cases . the soreness may last up to four days. The muscle soreness may be due to the damage in muscle and connective tissue.
3: Muscle Diseases/Disorders:
a: Atrophy:
Diseases and damages the Brain or nerves that stimulate muscles.
b: Muscular dystrophy:
Is a serious disease that directly affects muscles. It weakness the skeletal muscles.
BY: Aveenash
Thursday, March 23, 2017
HUMAN SKIN--- --Rizwan
HUMAN SKIN
- The Human Skin is outer covering of body. In Human it is largest organ of integumentry system.
DERMETOLOGY study of Skin.
- Skin with a total area of about 20 square feet.
- Human skin is simillar to that most of mammals, though nearly all Human skin is covered with hair follicles.
- Skin has a mesodermal cells, Pigmentation , such as melanin provided by melanocytes, which absorb some of potentially dangerous UV in Sunlight. It also contain DNA repair enzyme that help reverse UV damage such that People lacking these genes for these enzymes suffer high rate of skin cancer.
- The skin is largest organ of human body, for average adult human the skin has a surface area of b/w 1.5-2.0 square meter. The thickness of skin varies considerably over all parts of body, Men and Women, Young and Old. An example is the skin of forearm which is n average 1.3mm in male and 1.26 in female.
- The average square inch (6.5 cm2) of skin holds sweat glands, 20 blood vessels, 60,000 melanocytes and more than 1000 nerve endings.
SKIN HAS A THREE LAYERS
EPIDERMIS Layer
DERMIS Layer
HYPODERMIS Layer
- 1. EPIDERMIS layer:- Epidermis layer is outer most layer of skin, provides a water proof barier and create our skin tone.
- Epidermis contain no blood vessels (AVASCULAR) and cells in deepest.
- the main type of cells which make up epidermis are Markel cells, Keratinocytes, with Melanocytes cells are present.
- Epidermis is divided into FIVE sub-layers or strarta.
- 1: Stratum Corneum
- 2: Stratum Lucidum
- 3: Stratum Granulosum
- 4: Stratum Spinosum
- 5: Stratum Germinatium (also called stratum basale).
2: DERMIS Layer:- It is a true Skin made of Connective tissue and is a VASCULAR.
- It is a thicker inner layer of skin.
- matted masses of Connective tissue, Elastic Fibers, Nerve endings, Muscles, Hair follicles, Oil and Sweat glands.
- Dermis contain lots of sensory cells (heat, cold, pain, pressure).
3: HYPODERMIS Layer:- Subcutaneous. Attaches integument to muscle.
- It is a loose Connective tissue and FAT of body's store.
- Absorbs shocks.
- .
FUNCTIONS OF SKIN
- Cover-protects from germs, dehydration, injury.
- First line of Defense.
- Regulate body temperature.
- Manufactures Vitamin D.
- Site of many Nerve endings.
- Temporary storage of Gulucose, fat, water and salt.
- Protect from UV Radiations.
- .
ONE square cm of skin contains:
- 3,000,000 cells.
- 10 Hairs.
- 1 Yard of blood vessels.
- 4 Yards of nerves.
- 700 Sweat glands.
- 200 nerve endings to record pain.
- 3000 Sensory cells at the end of nerve fiber.
- .
DISEASE OF SKIN:
- ACENE:- A common and Chronic disrder of sebaceous glands.
- ATHLETE'S FOOT:- Fungal infection of the epidermis.
- DERMATITIS:- A nonspecific inflamation of skin.
- PSORIASIS:- Patches of raised. Redish skin,
- SKIN CANCER:-
- Associated with UV light.
BY: RIZWAN U-DIN CHANNA
Subscribe to:
Posts (Atom)