- The fetal blood reaches the placenta via the umbilical arteries, which are branches of the caudal aortic system. Well-oxygenated blood from the placenta is returned by the umbilical veins, about one-half passing through the liver sinusoids, and the rest bypassing the liver via the ductus venosus into the inferior vena cava system. The blood flow is regulated by a muscular sphincter in the ductus venosus, close to the umbilical veins. The blood then passes to the right atrium. Since the inferior vena cava also receives deoxygenated blood from the lower portion of the body, the blood entering the right atrium is not as well oxygenated as that in the umbilical veins
- The minor circulation (circulation through the lungs): although existing anatomically, the minor circulation is almost completely short-circuited by 2 major mechanisms
- THE BLOOD FROM THE INFERIOR VENA CAVA is directed largely by the lower border of the septum secundum, through the foramen ovale, which directs blood from the right to the left side of the heart. Here it mixes with small amounts of deoxygenated blood returning from the lungs via the pulmonary veins
- From the left atrium, blood goes to the left ventricle and out of the heart via the aorta to vessels of the head and neck, upper limbs, and the rest of the body. The former receive richer, well-oxygenated blood
- Some oxygenated blood from the inferior vena cava stays in the right atrium, mixes with deoxygenated blood from the superior vena cava and coronary sinus, and passes to the right ventricl Blood leaves via the pulmonary trunk and passes through the ductus arteriosus, which diverts it from the pulmonary to the aortic system
- Little goes to the lungs (?10%) due to pulmonary vascular resistance
- The mixed blood in the descending aorta (58% saturated with oxygen) passes to the umbilical arteries and is returned to the placenta for reoxygenation
- THE FETUS cannot use its pulmonary system since it lives in a liquid environment. The lungs, nevertheless, have been ready and prepared to fulfill their role from month 6 of pregnancy. It becomes effectively functional only when the fetus is born
- Circulation at birth: placental circulation is interrupted. The abrupt drop in intrathoracic pressure brought about by the first respiration (aeration of the lungs) helps contribute to the initial pulmonary circulation
- BLOOD PRESSURE decreases in the pulmonary artery even though its flow is increased since it supplies a capillary network considerably enlarged by expansion of the pulmonary parenchyma
- As a result, blood flow decreases (even reverses momentarily) in the ductus arteriosus; its walls contract, and in a few days, it closes off completely
- Closure appears to be mediated bybradykinin, released from the lungs during their initial inflation. Its action depends on the high oxygen content of the aortic blood resulting from ventilation of the lungs at birth
- Similarly, influx of pulmonary blood into the left atrium causes the septum primum to be pressed against the septum secundum, and the foramen ovale is closed
- The umbilical arteries also constrict at birth and prevent blood loss
- THE CIRCULATORY SYSTEM at this time-resembles its adult form, with separation of the minor and major circulations. Nevertheless, occlusion of the 2 circuits is still, for some time, only physiologic (functional)
- THE CIRCULATORY SYSTEM becomes fully anatomic after several weeks due to the proliferation of endothelial and fibrous tissue
- Fibrous degeneration of the ductus arteriosus forms the ligamentum arteriosum, between the left pulmonary artery and the concave inferior surface of the aortic arch
- Complete fusion of the septum primum to the septum secundum forms a definitive interatrial septum. Traces of the former passage, the foramen ovale, are seen as a depression, the fossa ovalis, in the right interatrial wall.
- The fetal blood reaches the placenta via the umbilical arteries, which are branches of the caudal aortic system. Well-oxygenated blood from the placenta is returned by the umbilical veins, about one-half passing through the liver sinusoids, and the rest bypassing the liver via the ductus venosus into the inferior vena cava system. The blood flow is regulated by a muscular sphincter in the ductus venosus, close to the umbilical veins. The blood then passes to the right atrium. Since the inferior vena cava also receives deoxygenated blood from the lower portion of the body, the blood entering the right atrium is not as well oxygenated as that in the umbilical veins
- The minor circulation (circulation through the lungs): although existing anatomically, the minor circulation is almost completely short-circuited by 2 major mechanisms
- THE BLOOD FROM THE INFERIOR VENA CAVA is directed largely by the lower border of the septum secundum, through the foramen ovale, which directs blood from the right to the left side of the heart. Here it mixes with small amounts of deoxygenated blood returning from the lungs via the pulmonary veins
- From the left atrium, blood goes to the left ventricle and out of the heart via the aorta to vessels of the head and neck, upper limbs, and the rest of the body. The former receive richer, well-oxygenated blood
- Some oxygenated blood from the inferior vena cava stays in the right atrium, mixes with deoxygenated blood from the superior vena cava and coronary sinus, and passes to the right ventricl Blood leaves via the pulmonary trunk and passes through the ductus arteriosus, which diverts it from the pulmonary to the aortic system
- Little goes to the lungs (?10%) due to pulmonary vascular resistance
- The mixed blood in the descending aorta (58% saturated with oxygen) passes to the umbilical arteries and is returned to the placenta for reoxygenation
- THE FETUS cannot use its pulmonary system since it lives in a liquid environment. The lungs, nevertheless, have been ready and prepared to fulfill their role from month 6 of pregnancy. It becomes effectively functional only when the fetus is born
- Circulation at birth: placental circulation is interrupted. The abrupt drop in intrathoracic pressure brought about by the first respiration (aeration of the lungs) helps contribute to the initial pulmonary circulation
- BLOOD PRESSURE decreases in the pulmonary artery even though its flow is increased since it supplies a capillary network considerably enlarged by expansion of the pulmonary parenchyma
- As a result, blood flow decreases (even reverses momentarily) in the ductus arteriosus; its walls contract, and in a few days, it closes off completely
- Closure appears to be mediated bybradykinin, released from the lungs during their initial inflation. Its action depends on the high oxygen content of the aortic blood resulting from ventilation of the lungs at birth
- Similarly, influx of pulmonary blood into the left atrium causes the septum primum to be pressed against the septum secundum, and the foramen ovale is closed
- The umbilical arteries also constrict at birth and prevent blood loss
- THE CIRCULATORY SYSTEM at this time-resembles its adult form, with separation of the minor and major circulations. Nevertheless, occlusion of the 2 circuits is still, for some time, only physiologic (functional)
- THE CIRCULATORY SYSTEM becomes fully anatomic after several weeks due to the proliferation of endothelial and fibrous tissue
- Fibrous degeneration of the ductus arteriosus forms the ligamentum arteriosum, between the left pulmonary artery and the concave inferior surface of the aortic arch
- Complete fusion of the septum primum to the septum secundum forms a definitive interatrial septum. Traces of the former passage, the foramen ovale, are seen as a depression, the fossa ovalis, in the right interatrial wall.

Thursday, April 13, 2017
Embryology: Circulation of blood before and after birth. By: Anmol Advani
Wednesday, April 12, 2017
Arches of Foot By Geeta goswami.
What is arch?
Longitudinal(i-e Sagittal plane) and transverse (i-e Frontal and hhorizontal planes) concavity of foot profile maintained by interlocking shapes of bones, plantar ligaments(i-e ligaments in the sole of the foot), plantar aponeurosis(plantar fasciai-e the thick connective tissue present on plantar side of the foot), tendons of extrinsic muscles and tension imposed by intrinsic muscle action.Bones involve in arches formation:
Tarsals bone: Metatarsals bone:
1)-Talus. 1st (medial) MT bone.
2)-Calcaneus. 3rd MT bone.
3)-Navicular bone. . 4th MT bone.
4)-Cuboid. 5th MT bone.
Plantar ligaments forming arches of Foot:
1)-Plantar plates.
2)-Metatarsal and tarsometatarsal ligaments.
3)-Long plantar ligament.
4)-Plantar calcaneocuboidal ligament.
5)-Plantar calcaneonavicular ligament.
6)-Plantar cuneonavicular ligament.
7)-Plantar intercuniform ligament.
8)-Plantar cuboideonavicular ligament.
9)-Plantar cuneocuboid ligament.
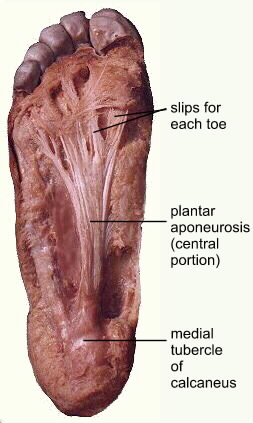
Planter aponeurosis:
Types of arches:
a) Longitudinal:
1. Medial.2. Lateral.
b) Transverse:
1. Anterrior.
2. Posterior.
Formation or structure of Arches:
Medial longitudinal Arch:
This arch is considerably higher, more mobile & resilient than the lateral. Its constitution isisas follows.Ends:
The anterior end is formed by the heads of the first, second and third metatarsals. The phalanges do not take part in forming the arches. The posterior end of this arch is formed by the medial tubercle of the calcaneum.
Summit:
The summit of the arch is formed by the superior articular surface of the body of the talus.Pillars:
The anterior pillar is long and weak.It is formed by the talus, the navicular, the three cuneiform bones, and the first three metatarsal bones. Posterior pillar is short and strong. It is formed by the medial part of the calcaneum.The major joint of the arch is the tarsocalcaneonavicular joint.
Lateral longitudinal Arch:
This arch is characteristically low, has limited mobility, & is built to transmit weight and thurst to the ground. This is in contrast to the medial longitudinal arch which act as a shock absorber. The constitution of the lateral longitudinal arch is as follows.
Ends:
The anterior end of the arch is formed by the headhead of the 4th & 5thth Metatarsal bones. TheThe Posterior end is formed by the lateral tubercle of the calcaneum.
Summit:
The summit lies at the level of the articular facets on the superior surface of the calcaneum at the level of the subtalar joint.
Pillars:
The anterior pillar is long and weak. It is formed by the cuboidcuboid bone and by the 4th and 5th metatarsals. The posterior pillar is short and strong. It is formed by the lateral half of the calcaneum.
Main joint:
The main joint of the arch is the calcaneocubiod joint.
Anterior Transverse Arch:
The anterior transverse arch is formed by the heads of the five metatarsal bones. It is complete because the heads of the first and fifth metatarsals both come in contact with the ground, and form the two ends of the arch.
Posterior Transverse Arch:
The posterior transverse arch is formed by the greater parts of the tarsus & metatarsus. It is incomplete because only the lateral end comes in contact with the ground, the arch forming a 'half dome' which is cmplete by a silimar half dome of the opposite foot.
Factors Responsible For Maintenance Of Arches:
In general, the factors helping in maintaining the various arches areare as follows.
1. Shape of the bones concerned.
2. Intersegmental ties or ligaments (and muscles) that hold the different segments of the arch together.
3. Tie bones or bowstrings that connect the two ends of the arch.
4. Slings that leep the summit of the arch pulled up. Each of these factors is considered below.
1. Bony Factor:
The posterior transverse arch is formed, and maintained mainly because of the fact that many of the tarsal bones involved (e.g. the cuneiform bones) and the heads of the metatarsal bones, are wedge-shaped, the apex of the wedge pointing downwards.
The bony factor is not very important in the case of the other arches.
2. Intersegmental Ties:
All arches are supported by the ligaments uniting the bones concerned. The most important of these are as follows.
(I) The spring ligament for the medial longitudinal arch.
(II) The long and short plantar ligaments for the lateral longitudinal arch.
(III) In the case of the transverse arch, thethe Metatarsal bones are held together by the interrosseous muscles also.
3. Tie Beam:
The longitudinal arches are prevented from flattening the plantar aponeurosis, and by the muscles of first layer of the sole. These structures keep the anterior and posterior ends of these arches pulled together. In case of the transverse arch, the adductor hallucis acts as a tie beam.
4. Slings:
a) The summit of the medial longitudinal arch is pulled upwards by tendons passing from the posterior comparment of the leg into the sole, I.e.tibialistibialis Posterior, flexor hallucis longus, flexor digitorum longus.
b) The summit of the lateral longitudinal arch is pulled upwards by the peroneus longus & peroneus brevis.
c) The tendons of tibialis anterior and peroneus longus together form a sling(or stirrup) which keeps the middle of the foot pulled upwards, thus supporting the longitudinal arches.
d) As the tendon of the peroneus longus runs transversely across the solesole, it pulls the medial and lateral margins of the sole closer together, thus maintaining the transverse arches. The transverse arch is also supported by tibialis posterior which grips many of the bones of the sole through its slips.
What is the function of Arches?
Arches of foot help in:
1)-Weight- bearing.
2)-Providing upright posture.
3)-Fast walking.
4)-Running.
5)-Jumping.
NOTE:-Foot print are not complete due to the arches.
Subscribe to:
Posts (Atom)